World AMR Awareness Week: Educate. Advocate. Act now.
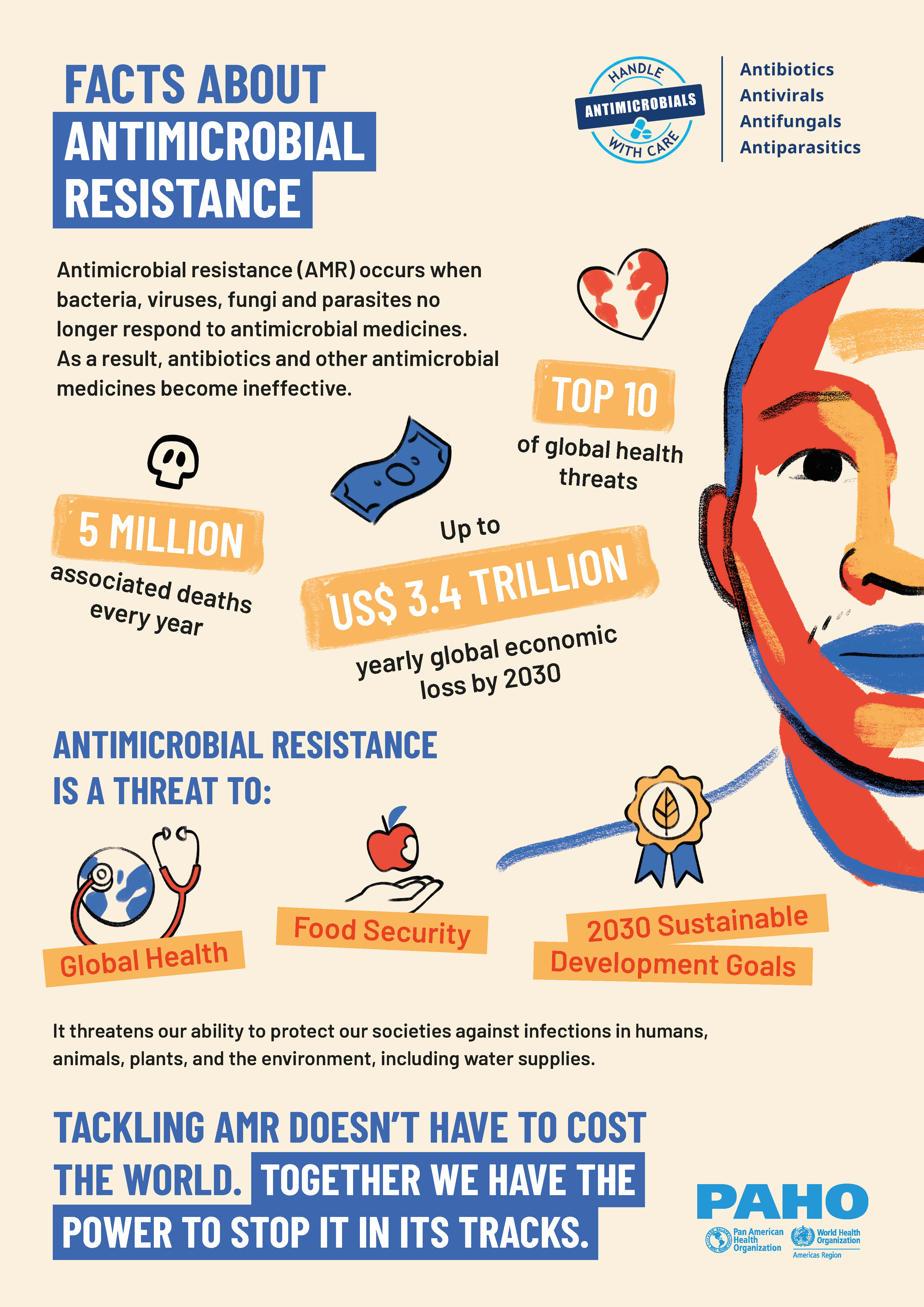
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi and parasites no longer respond to antimicrobial agents. As a result of drug resistance, antibiotics and other antimicrobial agents become ineffective and infections become difficult or impossible to treat, increasing the risk of disease spread, severe illness and death.
The World AMR Awareness Week (WAAW) is a global campaign to raise awareness and understanding of AMR and promote best practices among stakeholders to reduce the emergence and spread of drug-resistant infections. WAAW is taking place from 18-24 November.
© WHO
How is the University of Vienna contributing solutions to the AMR crisis?
Researchers from the University of Vienna, in collaboration with partners from a multidisciplinary consortium called ANTI-TB (Antibiotic Nanocarriers for Therapeutic Inhalation Treatment of Tuberculosis) recently published a study in the journal ACS Infectious Diseases reporting a possible new therapeutic approach in the treatment of multi-drug-resistant tuberculosis.
The team successfully reformulated bedaquiline, a second-line drug for tuberculosis (TB), into an inhalable liposomal nanocarrier. Liposomes are small spheres (100 nm in size; a thousand times smaller than a human hair) that are filled with the drug and help to keep the drug in the lung, where the TB bacteria are located. This innovative approach promises to improve the pharmacokinetic profile of the drug compared to its conventional oral form. By delivering higher concentrations of the medication directly to the lungs - the primary site of infection - it could significantly boost therapeutic efficacy against multi-drug-resistant TB.
Why tuberculosis?
Tuberculosis is the world's leading infectious disease caused by bacteria. The treatment of tuberculosis is made much more difficult by the alarming increase in cases caused by antibiotic-resistant pathogens.
"The use of inhaled nanomedicines has the potential to not only increase the effectiveness of bedaquiline against pulmonary tuberculosis, but also reduce a potentially harmful side effects."
says Prof. Lea Ann Dailey from the Department of Pharmaceutical Sciences, who led the study arm investigating the pharmacokinetics of the new formulation.
Researchers from the ANTI-TB consortium posed the question of whether novel nanomedicine-based drug formulations, like liposomes, could better reach the pulmonary infection sites and increase the concentration of the drug there when administered by inhalation. At the same time this way of administering bedaquiline could reduce drug-associated side effects in other parts of the body, such as the heart. The study results suggested that this was indeed the case. Liposomal bedaquiline applied directly to the lungs showed higher lung concentrations and an improved antibacterial effect, which is key to preventing drug resistance.
Their study also found lower levels of the drug metabolite, N-desmethyl-bedaquiline, in the blood, especially when compared to the orally administered drug. Since higher metabolite concentrations are associated with higher risk of cardiac side effects, the new therapeutic approach could extend bedaquiline treatment to patients who are at risk for these specific adverse effects. At the same time, the inhaled liposomal treatment may even improve the therapeutic effect compared to tablets, although further studies over longer treatment periods are required to confirm this.
The research team now hopes to build on these exciting findings by applying for further funding to expand their nanomedicine approach by assessing inhaled liposomal bedaquiline in the context of tuberculosis therapy.

© WHO
© PAHO
